Saving baby Beau: Finding strength in faith, family and the right medical team
- Category: Cardiology, Patient Stories
- Posted on:

Mary Beth Brown was a stay-at-home mother of two young boys, 2-year-old Elder IV and 3-month-old McCall, from Bush, Louisiana. After noticing some changes, she took a pregnancy test. Shock and realization set in when they saw those double lines.
“We started wrapping our mind around having ‘Irish Twins’,” said Mary Beth. “We were excited, but I started to miscarry at 11 weeks, on a Friday evening. I spoke with my OB, who advised that I would likely lose the baby over the weekend and walked me through what to expect. But things subsided and when I went into his office on Monday morning the baby’s heartbeat was strong and things normalized.”
At 12 weeks, she was referred to a maternal fetal medicine clinic that handled high-risk pregnancies.
“They kept a very close eye on the baby as further complications arose with the pregnancy. At 16 weeks, they did an early anatomy scan. It was during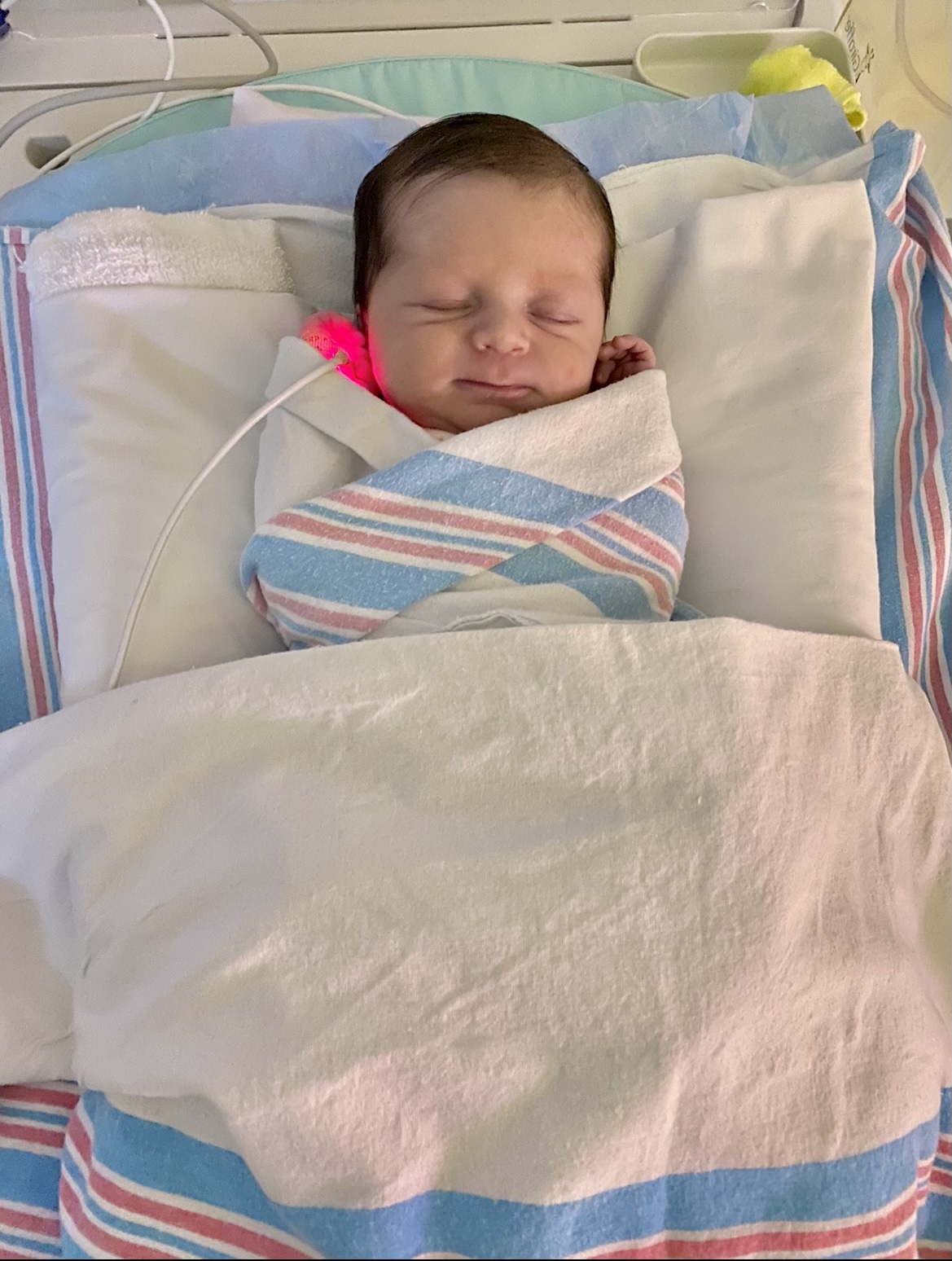 COVID, so my husband couldn’t join me at any of the appointments. During the scan, the tech and I realized that it was another boy and started laughing,” said Mary Beth. “Then suddenly, the tech stopped and got the doctor. He looked at the ultrasound, and then called in another doctor.”
COVID, so my husband couldn’t join me at any of the appointments. During the scan, the tech and I realized that it was another boy and started laughing,” said Mary Beth. “Then suddenly, the tech stopped and got the doctor. He looked at the ultrasound, and then called in another doctor.”
Without saying more, he asked for Mary Beth to meet him in the office. She called her husband so they could receive the news together.
DISCOVERING SOMETHING WAS WRONG
“He told us it’s too early to figure out what exactly this is, but it’s not good, and it’s not something that will fix itself,” said Mary Beth.
 The doctor explained her baby’s heart wasn’t developing as it should. It was smaller than the other organs and missing parts. After being referred to a specialty facility in Baton Rouge, they found multiple heart defects.
The doctor explained her baby’s heart wasn’t developing as it should. It was smaller than the other organs and missing parts. After being referred to a specialty facility in Baton Rouge, they found multiple heart defects.
“The specialist painted a very doom-and-gloom scenario and suggested terminating the pregnancy at 18 weeks. He told us he wouldn’t be a healthy baby and that a normal life would not be possible,” said Mary Beth. “We had two perfectly healthy children and knew nothing about heart defects.”
They decided to get a second opinion from an outside doctor who was able to narrow down his heart condition to either a Double Outlet Right Ventricle or Hypoplastic Left Heart Syndrome. From that appointment, Mary Beth and her husband, Elder, interviewed hospitals around the nation to find the best care for those two defects, which led them to Children’s Hospital New Orleans.
One of their first appointments was with Dr. Shannon Powell, a fetal cardiologist who was able to review the imaging and do new scans. Dr. Powell confirmed the diagnosis of double outlet right ventricle, ventricular septal defect with transposition of the great arteries and pulmonary atresia complicated by a hypoplastic right heart. Dr. Powell pulled a team together to begin putting a plan in place for their baby once he was born.
Dr. Thomas Kimball, Chief of Pediatric Cardiology and Co-Director of The Heart Center, Dr. Frank Pigula, Chief of Pediatric Cardiothoracic Surgery and Co-Director of The Heart Center (who joined Children’s Hospital from Boston in January 2021) and pediatric cardiologist Dr. Shannon Powell collaborated for the baby's care.
“We wanted to ensure we had the best medical team possible, and all signs pointed back to Children’s Hospital. Not only was Children’s Hospital the most convenient, but it was also a clear fit with Dr. Kimball and Dr. Powell. Dr. Kimball was very reassuring with an exceptionally warm bedside manner.”
For the best access to care, her medical team recommended she deliver at Touro LCMC Health.
“Dr. (Stephen) Hales held our hand throughout the entire process. He reviewed scans with us and was an incredible source of knowledge. He provided peace of mind and expertise in caring for a special needs baby with two other young children. I was experiencing self-doubt as to how I would handle Beau’s diagnosis and care for the rest of my family but Dr. Hales quickly eliminated the fear and replaced it with love and support." shared Mary Beth, "This diagnosis was agonizing. It’s like going to sleep, knowing we were going to have a nightmare that we couldn’t change anything about. We prayed every day for strength, knowledge and for our medical team, who were guiding us through this.”
During that period, Mary Beth and Elder explored and researched Children’s Hospital and its various departments and read blog posts of other families going through similar situations.
“I felt comforted by this, knowing he was going to have the best doctors working on his case every step of the way, whatever challenges we may face. We are fortunate that his defects were identified early on, and we could prepare in every sense of the way: medically, personally, and spiritually.” said Mary Beth.
BIRTHING BEAU
At 39 weeks, Mary Beth scheduled the delivery at Touro LCMC Health for January 13, 2021. Her family chose that date because it’s also his paternal grandmother’s birthday. Five hours after receiving Pitocin, Beau was born weighing 7.9 pounds, delivered by Dr. Rebecca Perret.
“We had a remarkable medical team. Beau came out breathing and pink, so we were able to hold him and quickly pray over him before they took him away,” said Mary Beth. “It was a blessing he came out as big as he did because we could bypass additional complications of a low-weight heart baby.”
Beau was taken to the NICU to stabilize before being transferred to Children’s Hospital via helicopter two hours later. Beau was born with a whole host of heart issues including Double Outlet Right Ventricle (DORV) Dextro-Transposition of the Great Arteries (d-TGA), pulmonary atresia, hypoplastic right ventricle (HRV), Large Inlet VSD with Outlet Extension (better known as a hole in heart), central Pulmonary Artery Hypoplasia and overriding and straddling tricuspid valve with a single coronary artery.
Which is all to say, the heart could not pump blood to his lungs, which means he could not oxygenate the blood going to the rest of the body. He also had a unique hole in his heart.
“The second time we saw our baby was to say goodbye. He was wrapped up in blankets with different lines in his body. They set him up in this large transport contraption to keep him stabilized for the flight over to Children’s Hospital. My husband followed him, and I was discharged that same evening so that I could join them on the CICU floor at Children’s. My recovery was placed on the backburner but I was familiar with what to expect so Beau’s medical needs could stay paramount.” said Mary Beth.
It was important to Mary Beth and Elder that Beau not be alone on his first day of life, and Mary Beth was relieved when she arrived at Children's Hospital to see doctors and nurses interacting with him in the same manner she would have.
“It meant a lot that they understood that. Children’s provided exceptional care from day one. We could not have asked for a better team of nurses.” said Mary Beth.
During this time, doctors developed a plan for Beau’s first surgery. At three days old, Beau was put under anesthesia for a catheterization laboratory, commonly referred to as a cath lab. It’s an examination room with diagnostic imaging equipment used to visualize the arteries of the heart.
“That was scary, but he did great. His procedure prepared everyone for his upcoming surgery, and doctors were able to get the pictures they needed,” said Mary Beth.
Beau was a complex case. He formed a large hole in his heart, but his body adapted by having his arteries grow through it. Beau’s first of three big surgeries was a Norwood procedure. For the next four days, the family and medical staff worked together to make sure he was stable as possible.
“It was important for me to attempt to nurse him. Most heart babies can’t nurse because the ‘suck, swallow, breathe,’ technique is difficult to master when the heart doesn’t pump normally, but I wanted to at least try. He took immediately,” said Mary Beth. “But when a doctor was skeptical, Dr. (LaTasha) Lewis stepped in, allowing me to continue. She was supportive of us, taking the time to check in every day. She had such a positive influence on our experience at Children’s, especially those initial few weeks. She fought for our baby and trusted that I knew what was best for him.”
Beau was getting bigger and healthier in that time, gaining almost a whole pound in his first six days of life, weighing 8.5lbs right before surgery.
Dr. Frank Pigula, who was to perform the surgery, was incredibly helpful through the whole process. “He was very forthright with us on what to expect, from the possible complications to timeline of recovery after surgery. It was something we would always remember because Beau was his first patient at this hospital. He was so personable and caring, putting our fears at ease and answered all our questions. So, when the time did come to say goodbye to Beau for surgery, I felt as much peace as I could knowing we did everything possible to put him in the right hands,” said Mary Beth.
THE INITIAL PROCEDURE
Dr. Pigula performed a central arterioplasty and placed an aortopulmonary shunt in five hours. Mary Beth was on pins and needles, holding tight to the consistent updates from the surgical team via the hospital’s app. After the procedure, Beau’s chest was kept open due to inflammation and swelling.
“Walking in to see our new baby on a ventilator was devastating. He had 25 to 30 lines hooked up to him. He couldn’t breathe or move on his own,” said Mary Beth. “It was gut wrenching to see him like that. He couldn’t move, cry or make any sound during that time.”
Beau recovered well while being on the ventilator for about a week; however, being stagnant for so long took its toll, creating another challenge for Beau.
“After he woke up, he lost all memory of how to suck, swallow and move. Most of his natural instincts were forgotten. We had physical and occupational therapists come in multiple times a day to help regain function and CICU RN, Sarah Lass, made a world of difference in everyday care for Beau,” said Mary Beth. “Feeding him, changing him, holding him… all of it changed.”
One month after baby Beau was born, he was finally able to go home. The family received help from a home monitoring team, Stephanie Bush, NP, and Lynn Bardales RN.
“We would have been lost without Stephanie and Lynn. They provided an immense amount of knowledge, reassurance and guidance at all times,” said Mary Beth.
THE GLENN PROCEDURE
 At five months old, Beau had doubled his birth weight at a healthy 18 pounds. Dr. Pigula prepared him for his next surgery, called the bi-directional Glenn procedure. This surgery was also five hours, but the recovery was much faster this time around.
At five months old, Beau had doubled his birth weight at a healthy 18 pounds. Dr. Pigula prepared him for his next surgery, called the bi-directional Glenn procedure. This surgery was also five hours, but the recovery was much faster this time around.
“Dr. Pigula said that was one of the most perfect Glenn surgeries he had ever performed. There were no complications, and he was able to tolerate being taken off the ventilator in the matter of a few hours,” said Mary Beth. “He did experience some intense headaches, but they passed in a day or two.” Beau was discharged 4 days after surgery.
It’ll now be several years before his third open heart surgery, the Fontan procedure. “We still have a long road and our doctors have warned that there will be hard times ahead, including the most intense and invasive surgery of the series. We pray daily for guidance for our family and his medical team as we navigate these next few years together.”
“Right now, we’re in what they call ‘the honeymoon period.’ We have regular cardiology visits with Dr. Steffan Sternich and nurse Alli Carter every six months, where he receives a full workup with the EKG and blood labs,” said Mary Beth. “So far so good, everything looks stable and healthy. Beau is doing extremely well.”
Beau has also been hitting all his major milestones along the way. At two years old, he’s tipping the scales at 33 pounds, putting him in the 98th percentile.
“Beau is a big boy on any ratio. He loves to eat and is so happy. He hasn’t shown any delays and is developing on the normal curve like any other regular child which is a miracle in and of itself considering the amount of time he was on the bypass machine. He’s such a joy to be around and brings a level of happiness to our family I could have never imagined,” said Mary Beth. “It’s as if he knows something beyond his control is going on. I’m confident he’ll always maintain a positive and uplifting disposition no matter what he encounters in life.”
regular child which is a miracle in and of itself considering the amount of time he was on the bypass machine. He’s such a joy to be around and brings a level of happiness to our family I could have never imagined,” said Mary Beth. “It’s as if he knows something beyond his control is going on. I’m confident he’ll always maintain a positive and uplifting disposition no matter what he encounters in life.”
With his condition, Mary Beth says Beau will always be more restricted on types of activities he can do, but he’s not letting that stop him from exploring. Beau loves chasing after his big brothers, swimming and playing outside at his family’s country home.
“At first, we kept Beau’s diagnosis very quiet to give us time to process and make the best decision for our son. Now that we’re more experienced, we realize Beau didn’t go through this for us to keep this private. My hope is for Beau’s journey to encourage other parents who are just starting their own heart journey. It’s important for people to see that good things can happen- that there are success stories. It will seem like your world is falling apart, but a year later you can have this healthy and happy child, with the help of a great medical team. I can’t thank the team at Children’s enough,” said Mary Beth. “Little things seem so trivial to us now. Going through this experience, seeing your child fight for their life, makes every day with Beau a miracle. These trials have reshaped our family and we’re closer and more present with each other. Quality times together mean so much more to us now and our faith is stronger than ever.”
To learn more about the Heart Center at Children’s Hospital New Orleans, please visit: https://www.chnola.org/our-services/heart-center/.