Content
Discharge Instructions: Caring for Your Jackson-Pratt Drainage Tube
Your healthcare provider discharged you with a Jackson-Pratt drainage tube. They commonly leave this drain within the abdomen and other cavities after surgery. It helps drain and collect blood and body fluid after surgery. This can prevent swelling and reduces the risk for infection. The tube is held in place by a few stitches. It's covered with a bandage. Your healthcare provider will remove the drain when they determine you no longer need it.
Home care
Don’t sleep on the same side as the tube.
Secure the tube and bag inside your clothing with a safety pin. This helps keep the tube from being pulled out.
Empty your drain at least twice a day. Empty it more often if the drain is full. Wash and dry your hands before emptying the drain.
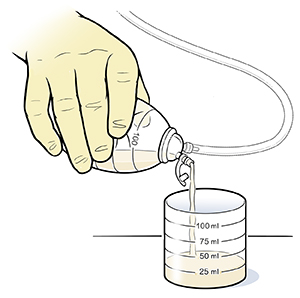
Lift the opening on the drain.
Drain the fluid into a measuring cup.
Record the amount of fluid each time you empty the drain. Include the date and time it was emptied. Share this information with your healthcare provider on your next visit.
Squeeze the bulb with your hands until you hear air coming out of the bulb if your healthcare provider has instructed you to do so (sometimes the bulb is used as a reservoir without suction). Check with your healthcare provider about specific drain instructions.
Close the opening.
If you are to change the dressing around the tube, follow the directions your provider has given you. Some dressings may not need to be changed, but your provider will let you know. Here are some general steps to follow:
Wash your hands.
Remove the old bandage.
Wash your hands again.
Clean the skin around the incision and tube site as instructed.
Put a new bandage on the incision and tube site. Make the bandage large enough to cover the whole incision area.
Tape the bandage in place.
Talk with your healthcare provider about showering with the drain. You may need to keep the bandage and tube site dry when you shower. Ask your healthcare team about the best way to do this.
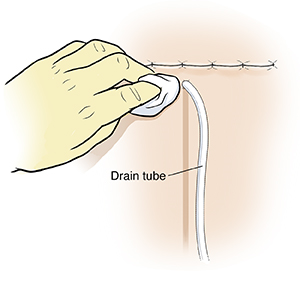
“Stripping” the tube helps keep blood clots from blocking the tube. Ask your healthcare team how often you should strip the tube. Stripping may not be needed, depending on where and why your healthcare provider placed the tube. It may even be dangerous in some cases.
Hold the tubing where it leaves the skin, with one hand. This keeps it from pulling on the skin.
Pinch the tubing with the thumb and first finger of your other hand.
Slowly and firmly pull your thumb and first finger down the tubing. You may find it helpful to hold an alcohol swab between your fingers and the tube to lubricate the tubing.
If the pulling hurts or feels like the tube is coming out of the skin, stop. Begin again more gently.
Follow-up care
Make a follow-up appointment as directed by our staff.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
New or increased pain around the tube
Redness, swelling, or warmth around the incision or tube
Drainage that is foul-smelling
Vomiting
Fever of
100.4 °F (38 °C) or higher, or as directed by your providerChills
Fluid leaking around the tube
Incision doesn't seem to be healing
Stitches become loose or the drain starts to come out
Tube falls out or breaks
Drainage that changes from light pink to dark red
Blood clots in the drainage bulb
A sudden increase or decrease in the amount of drainage (over 30 mL)